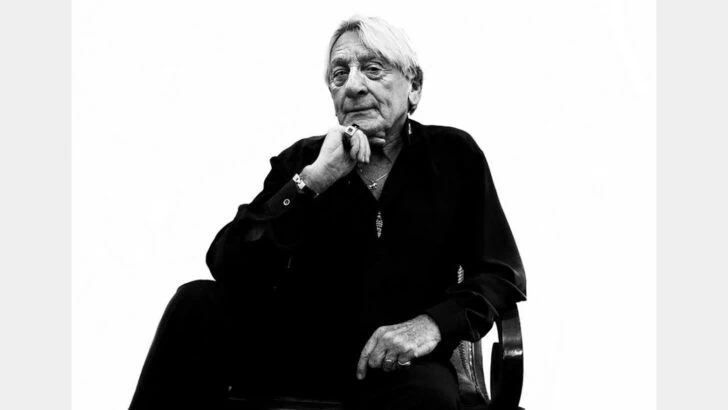
Robert Palmer is the lead adviser and specialist psychotherapist for the Burrell Street sexual health clinic. He spoke to us about gay men, drugs and why they’ve recently ran an advertising campaign advising to ‘SLAM SAFELY’.
By Patrick Cash
Tell us a little bit about yourself.
So I am the lead adviser and specialist psychotherapist for the unit and I’ve worked here for about eleven years. We opened Burrell Street about a year ago and we see about 60,000 patients a year. Which is a lot. And, as you might be aware, we’re the only service that’s open seven days a week, so Saturdays and Sundays are really quite interesting for us and incredibly busy as well.
Do you get a lot of people coming in at the weekend looking for PEP?
Definitely, yeah. We get a lot of people coming in looking for PEP, a lot of people who are quite wired still, from the night before, going to the sex parties, things like that, or going to the clubs. So it’s a very interesting Saturday and Sunday and there’s a lot of PEP definitely being given out to people as they kind of come down and realise what they might have done over the weekend.
I can imagine. And how did you get into sexual health yourself in the first place?
I’ve been around for quite a long time. I started in the early 90s, and I started as a health advisor in Newham. And in those days Newham was like a war zone, so the job was literally going from bed to bed to bed telling people they had HIV and of course there was no medication at that time, and sadly everybody was dying, so it was pretty awful at the time, and a pretty heavy introduction to this kind of work. But things have now changed, and I’ve always enjoyed working in sexual health – I have a private practice as well, which is all about sexual health – and there’s nothing better than going to work and talking about the most intimate details of somebody else’s life. I think it’s a really unusual and it’s a very intimate job, and I think it’s very special to have people sharing that kind of information with you.
I think, from my experience, a lot of sexual health workers seem to do it as a job but also there’s an element of caring about the community as well.
Absolutely, yeah. And that I think is really important, things have shifted, but when I started in the 90s, working with gay men in the NHS – it was still, partners were not recognised, or you didn’t talk about your sexuality when you went into a clinic and it was really, really hard. And I hope that I and lots of other people have contributed to making it much easier for the LGBT community to use the NHS in these kind of spaces.
How do you feel your role has changed with your current role as the head of Burrell Street, has it taken you more out of primary patient care?
I’ve made sure that it hasn’t. I lead the health advisor team and they’re also psychotherapists as well, and I lead all the results services as well, but I still make sure that there is at least one session a week where I’m still seeing the patients, because if you don’t do that I think you can lose track of what’s going on and what’s needed.
Okay, and just a couple of questions about Burrell Street: what was the vision for Burrell Street when it was put together?
The vision was to put take it out of a hospital setting and bring it into a community setting so that it was more accessible because most GU clinics are still at the back of hospitals and things like that, apart from maybe us and Dean Street. So we believed that it was time to just find a space that would be fresh and new and interesting to be in as well, so we got hold of architects who had never worked for the NHS before, so that their vision would kind of match with ours –
[Katrina, with blue hair, brings in coffees]
Thank you, Katrina!
[Katrina leaves]
She seems lovely.
She is.
And I suppose you want have that ethos here of having – not unprofessional, but a less corporate environment where people are free to have blue hair etc.
Well absolutely, and we want to make this place as relaxed as possible, which is why we’ll never charge for coffees, there’s wifi, there’s music, it’s all quite chilled out, with art, as well. I mean the art is really, really interesting, because it covers three international artists who work for us, and it was all provided by Guys and St Thomas’ charity, which has an arts section that provides art in hospitals that has really funded all of this for us. I think really, it’s beginning to attract a lot of gay men, this clinic, which is one of the things we wanted to do because we recognized that actually this is where we’ve got the highest rates of infection and we needed to do something about it.
And moving on to doing something about it… What was the thinking behind the current ‘Slam Safely’ campaign?
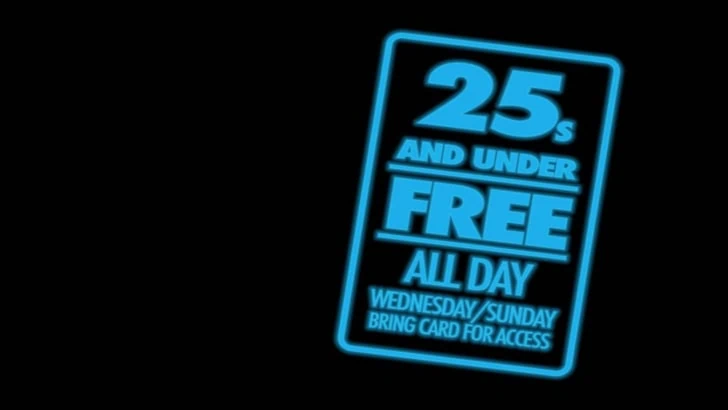
It comes off the back of a number of things, and the first thing is the number of injectors that we started to see at Burrell Street and we were really surprised. Because it kind of came out of nowhere. I think it’s been a very interesting history in the change of the use of the types of drugs that gay people are using, and I recognise that part of that is due to the closure of routes of certain types of drugs being able to get into the country, so people have had to change because of that, the influence of the legal highs in recent years as well, and the way that market has changed. But also there has to be something going on around the sex that people are having, and the headspace in which they are in, in order to choose the drugs that they are using and we didn’t expect to see such a rise in crystal meth use. We’re more surprised by the injecting of mephedrone. And what we seem to be seeing, and this is only anecdotal evidence for us, is that it’s an older age group that are injecting crystal, and it’s a much younger age group injecting mephedrone, which is why we’ve been targeting Grindr, yourselves and Boyz in particular.
Do you think the younger age group inject mephedrone because they see it as more harmless, even though it’s still injecting?
Yes. And because it’s very, very cheap as well, and they’re probably used to snorting it, or mixing it up in water and drinking it, and so will then probably get introduced to the idea of injecting it by a sex partner or at a sex party and will give it a go. The problem I have with mephedrone is it’s a nasty drug.
In what way?
The evidence and research we have around this drug and what it might do to people in the short and long-term is very, very small. This is not ecstasy where we’ve got a huge amount of data done over the years as to what kind of effect this drug will have, and it came out and hit a market at a very specific time to do a very specific thing, because the precursors of ecstasy were not available at that time. It’s very, very clever. But it has unpleasant side effects; the anxiety and the comedowns people get from it. They’re also injecting something that they’re buying from a dealer and they don’t know what is in that power or what they have to put in their bodies, and that concerns me as well.
Just to do a little bit of scientific context, what you snort what is the difference between that and injecting? When you inject you hit the bloodstream quicker and how does that affect the brain?
When you inject you hit the blood stream quicker, within a couple of seconds it’s kicking in –
And that affects the dopamine receptors?
Absolutely, yeah. And it must do something to the serotonin receptors as well I’d imagine. So you’ve got that kicking in but you’re going to get a different effect through the route in which it comes into the body. So if you snort it, you’re going to get high but you’ll lose some of the powder and it’ll get into the blood stream through being absorbed by the membrane but the high might last for a short period of time than perhaps if you’re ingesting it, and of course if you’re injecting it you’re not losing any of the drug and you’re getting the full extent of it.
Do you think the ‘slam safely’ ads, with the huge words saying ‘SLAM SAFELY’, might seem to condone slamming?
I don’t think so, I think we’re very clear actually about what we’re trying to say, which is: ‘if you must inject, then please do it safely.’ And I think we’re very clear about the wording that we use and being very, very careful on that as well. It’s not something that we want people to do and we’re not trying to advertise this as a service where it’s okay. We’re really concerned about the health of people. But this is a harm minimisation approach, and if I said to you ‘stop using’, that won’t do anything, it’s a typical psychological response, if I tell you to not do something you’ll want to do it more, so actually that’s not the right route to go down. How many years have the government been doing ‘stop taking drugs’ or ‘saying no’ and it doesn’t work. So what we do is have the ability to build up relationships with people who are using, and we know that gay men prefer to come to sexual health clinics and have a checkup and pick up things like needles rather than they would going to a community drugs team. They feel more comfortable here.
What about the younger generations who aren’t coming to Burrell Street and they’re just flicking through the pages and they just see the two words ‘Slam Safely’, but you think at least they’ve got that message?
Absolutely, which is ‘look after yourself’. And that’s what we want to put forward: if you’re going to do this, if you have to do this, for fuck’s sake, look after yourself in doing it. And what we do is provide syringes that are colour-coded, so if you’re at a party, you are not going to mistake your syringe for somebody else’s syringe. Because this is the perfect storm, you have a sex party where there’s a large number of people: there may be people who are HIV positive, HIV negative, Hepatitis C positive, Hepatitis B positive, and it becomes a perfect storm of sexually transmitted infections, injecting drugs and viruses and bacteria. What we want to do is try and limit the possibility of infections spreading.
You don’t think there’s a chance of this wording, or the vernacular used, of normalising the idea of slamming in a way?
I think that’s a really, really good question. But what we’re trying to do is make it, I suppose, words that people know. It’s like when we talk in the clinic: we start talking about people having sexual intercourse, they often don’t know what we mean, if we talk about fucking, people know exactly what we mean. And I think it’s the same with the vocabulary we use around slamming, people know what slamming is – if we’re talking about injecting, it becomes much more difficult language to start describing, so that’s why we’ve gone for this kind of wording.
What was the meeting like where you were decided on the ad, were some people really pro this message or were some people really anti, how did you come up with it?
How did we come up with it? I suppose we wanted something that was short, sharp, and to the point. What we know in marketing and advertising is that you can’t use a lot of wording and you’ve just got to hit people and that’s what we wanted to do. But I think we’ve chosen the right way forward, it’s been backed by the operations team and by the hospital’s communication department.
Okay, cool. And what statistics and figures are you having to deal with at Burrell Street?
I can’t tell you right now! I can tell you we’re giving away hundreds of slamming packs but I couldn’t right off the top of my head, I could not give you numbers because I haven’t got that data recently.
Sure. But it’s enough to have spurred on this campaign.
Yeah, first of all, we needed people to know that this service is here and that was the important thing so in a sense it’s become a service where you let people know and they come. Before that we were just kind of giving people needles as necessary, but now providing a pack actually makes much more sense.
Do you have a specific drugs counsellor here like David Stuart at 56 Dean Street?
No, we don’t work in the same way. We have one of the health advisors who has a specialist interest in drugs and alcohol, but as a team of advisors who are providing counselling and therapeutic interventions, all of them have had drugs and alcohol training, but we recognize that you don’t do things in a vacuum – everything connects with everything else. And there are reasons why we choose certain types of drugs, the ways we administer them, where we do them, and what we do them for. And so what we have is a kind of more holistic approach that starts by looking at the person and their sexuality and what’s going on in their lives and questions why they’re doing what they’re doing now. So we don’t feel we need to have a specific drugs worker, as all of them are available to deal with psychotherapy.
And in your opinion why do you think slamming has become so popular amongst ‘msm’ (men who sex with men) in recent years?
Why has it become so popular? I think it’s, like we were saying, it’s about what is available now. And I think it has to do with where our heads are as gay men at this time and the way in which we need to sometimes get out of it.
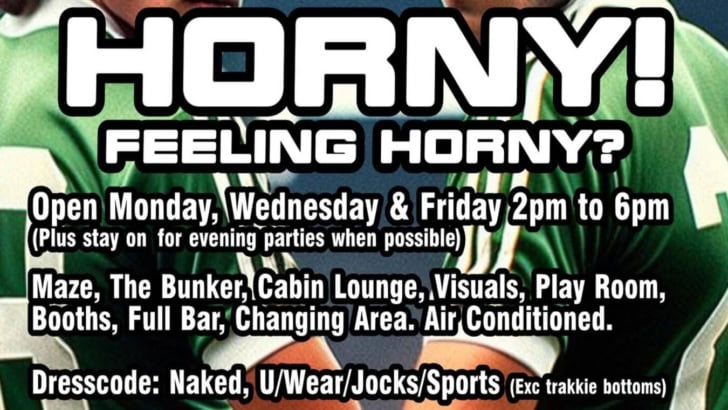
That’s my final question, do you have any theories yourself in general as to why gay men are practising chemsex to such an extent right now?
I think we do have very great difficulties around intimacy, and I think it’s like a McDonald’s: chemsex is a really quick way of becoming sexualised, feeling very, very horny, feeling connected to the person that we are with for that period of time. But the thing is, like McDonald’s it’s not very good for you, it leaves you feeling hungry afterwards and actually sometimes it’s worth considering preparing a really healthy meal and enjoying it slowly, and I feel we don’t do that very often. And that’s not necessarily our fault at all, it is the way we’ve been brought up, the way in which we still do not fit into this society, the way our parents have brought us, the relationships we had at school, the lack of sex education, HIV, all of these things kind of come together to make us who we are, and I think the homophobia that we’ve experienced as a community over the years can often be psychologically devastating and I think we turn it in on ourselves sometimes.
Do you think that Section 28 might have had something to do with it?
I’m sure all of those things did.
This is probably the hardest question, and final, final question, but how do you think we can move forward to find a solution?
I think having services that provide counselling and psychotherapy are really, really useful, but I think it’s a very interesting point regarding HIV at the moment, with the possibility of PrEP coming along so it changes the way in which we have sex yet again and it reminds me of the 70s before HIV came along, it feels like we’re moving to that point again.
That would be great, but we’re not addressing issues in that way, we’re just putting something in the mix that is enabling people to have condomless sex, we’re not addressing the deep-seated, deep-rooted issues, are we?
Well, no. I suppose you’re right. This is I think, for us to become a more healthy community is going to take a lot of looking after ourselves and realising that we are actually quite fragile, vulnerable people and have been through a war over the last twenty or thirty years, and we need to start pulling ourselves together. And actually as a response, as a community, the one we had to HIV is probably very similar to the way we need to start thinking about chemsex.
Burrell Street Clinic is the only sexual health clinic in London open seven days a week, and is located at 4-6 Burrell Street, SE1 0UN.